Delivery of telerehabilitation using advanced technology, and potentially exercise equipment, requires specific equipment and infrastructure needs. Refer ‘equipment’ and ‘local factors’
Staffing
There are currently no standardised ratios for patients to staff when delivering telerehabilitation using advanced technology. Anecdotally, health professionals with experience delivering telerehabilitation via videoconferencing report 1 clinician to 4-6 patients per session represents a comfortable group size to enable appropriate monitoring, exercise progression and ensure safety. Beyond rehabilitation delivery, clinicians have repeatedly identified the need/benefit for appropriate support for technology-based equipment and trouble-shooting.
“As far as staff goes, if you’re doing a Zoom class, you still really need to have the staff available, because, if you’ve got one person demonstrating the exercises, you have to have a spotter to actually look at the people that are doing exercises and make sure everything’s looking okay.”
- Quote from interview with health professional
Staff training
There are no formalised training programs for the delivery of telerehabilitation making use of advanced technology. Health professionals experienced in delivering pulmonary rehabilitation have identified that clinicians would ideally have experience of face-to-face pulmonary rehabilitation delivery before undertaking telerehabilitation. The potential to buddy or shadow a more experienced clinician before embarking upon independent service delivery may be helpful. Being confident and competent in managing technical issues, handling emergencies, delivering and progressing exercise training, and communicating are key skills identified by health professionals that would support clinicians to deliver effective telerehabilitation.
“Clinically prepared staff members are very important. I think experience is huge. It [telerehabilitation] could be done with less experience but you would need a very good manager of those less-experienced people."
- Quote from interview with healthcare professional based in U.S.
“Training is required. Either through proper sessions or shadowing and then learning in order to cater to the needs of the patient."
- Quote from interview with healthcare professional based in India
- For additional details on program delivery and processes see Program Delivery and program forms.
- For information on the delivery of telerehabilitation using a telephone based model see here.
Local factors
Equipment
Technology requirements – clinicians
To provide real-time supervision of exercise training both clinicians and patients need access to a suitable device, including webcam and microphone/speakers, to enable two-way audiovisual communication.
Being able to see and hear each other clearly is a fundamental component of telerehabilitation delivered using advanced technology.
Clinicians would ideally have access to a multi-screen set-up to enable visulisation of patients as well as access to relevant supporting materials e.g. patient medical record, safety contacts.

Video conferencing platform
The video conferencing platform may be dictacted by local resources or requirements. Key considerations for platform may include:
- suitability for group format
- ease of participant use/access
- cost of licence (or time limits/band width limits imposed by free software)
- ability to control/authorise participant access to the group
- HIPPA compliance (https://www.hhs.gov/hipaa/for-professionals/privacy/index.html)

Technology requirements – patient
To participate in telerehabilitation patient participants will need access to the following technology:
Device – a PC, laptop, tablet or smartphone. The device chosen will ideally allow patients to see all participants in the group and the clinician, which in some circumstances may make a smartphone screen too small. In addition, it may be necessary for the device to placed in a specific location relative to where the patient is exercising.


Camera – built into smartphone or tablet, may be built in or attached to laptop or PC
Microphone and speaker – usually built into the device. In some circumstances an external headset may improve sound quality however the ability to safely exercise whilst attached to the headset and device needs to be considered.
Video calling software (e.g. Zoom) that is compatible with your device. Patients will need to be advised ahead of time the platform to be used and provided details on how to access this. If using a smartphone or tablet it may be necessary to download/install an app first – some patients will find this step easier if they have the support of a staff member or family member. Where in-person assessments are possible, asking potential telerehabilitation participants to bring along their device to support installation of software and practice use of the platform may help to overcome future technology issues. Where this is not possible, clear step-by-step pictorial instructions for how to access the videoconferencing platform should be provided.


Telephone – A mobile or landline telephone to use in the event of technology failure or health concerns.
Exercise equipment

Telerehabilitation equipment as used in the REACH model comprising a step-through exercise bike, tablet computer with mobile data and pulse oximeter for monitoring. The tablet computer is affixed to a stand to enable clear two-way audio-visual communication for participant and healthcare professional and viewing of monitoring equipment. All equipment was commercially available.
Equipment considerations
Depending on resources and local clinical context, equipment may or may not be required and or provided for the delivery of telerehabilitation. For information on low resource telerehabilitation models see here. For telerehabilitaiton models making use of equipment and technology consideration needs to be given to:
- who provides/cost of equipment;
- how equipment is stored and transported;
- the physical footprint of equipment relative to the home environment;
- availability of stable internet and data usage costs.
Where participants have their own exercise equipment and/or device for videoconferencing it will be important for the clinician to determine appropriate set-up during the home visit to ensure adequate monitoring can be undertaken during exercise training ie. camera positioned approriately to see patient and/or monitoring equipment.

Storage
Cleaning protocols
Delivery plan
"The service was brilliant. The chap delivered it, he contacted me via my phone. Made sure it was okay to come."
- Quote from patient with COPD participating in telerehabilitation
WiFi/Internet access
Safety considerations
Emergency plan
Pre-determined emergency procedures should be developed in accordance with clinically appropriate decision making and local policies. Emergency protocols should be available to all clinicians during training for telerehabilitation service delivery and during all participant rehabilitation sessions. Emergency protocols may include advice or action:
- to not exercise;
- to contact their local GP/medical provider;
- to call for emergency services.
An example of an escalation flow chart can be found here.
Situations that require calling for emergency assistance immediately may include:
- Persistent Chest Pain
- Cardiac Arrest
- Heart Palpitations
- Numbness or slurred speech
- Fall where patient becomes injured and/or cannot get up
- Low oxygen saturation that does not improve with rest
- Severe breathlessness that does not improve with rest
- Severe Pain
- Severe allergic reaction or alcohol withdrawal
- Suicidal ideation, hallucinations or altered conscious status
- Uncontrolled bleeding or severe burns.
Participant contact list
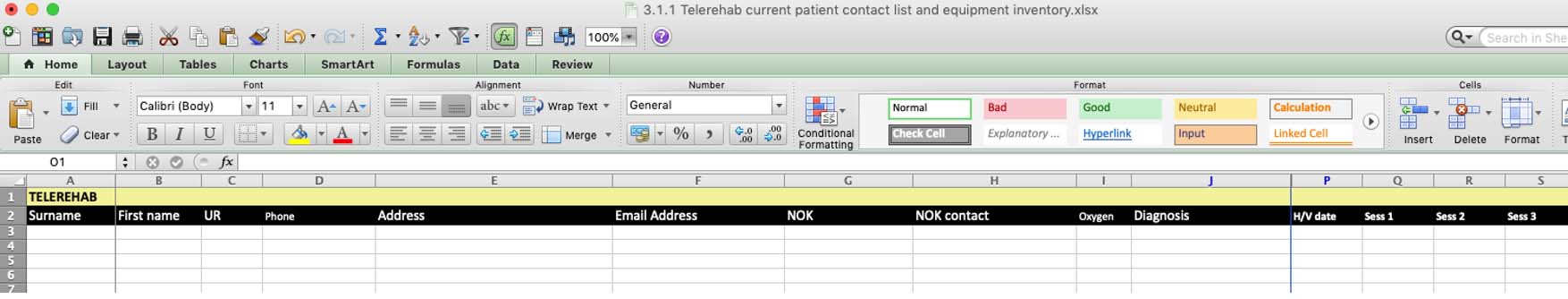
Example of list format for participant contact details, to be readily accessible to clinicians during telerehabilitation training, if required for emergency management.
Local emergency contact
All clinicians involved in the delivery of telerehabilitation should be familiar with local emergency procedures and the contact for emergency services in their area.
"We made sure the patient had someone around who could call 911 (emergency services) if they had to. We even went as far as if it was an outlying community and I knew there was a firehouse down the street from where the patient lived, we'd get the patient give them a heads-up 'I’ll be exercising at these times, so if a 911 call goes through, this is what it’s gonna be for!"
- Quote from interview with healthcare professional in the U.S.